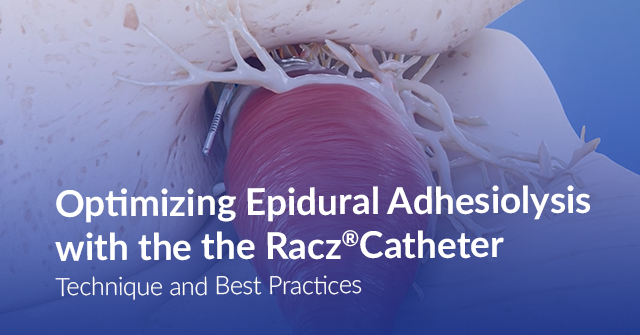
Epidural Adhesiolysis, also referred to as the Racz Procedure or Epidural Neuroplasty, is an interventional technique designed to mechanically and chemically disrupt epidural scar tissue that restricts nerve mobility and limits the spread of therapeutic injectates. Since its introduction by Prof. Gabor B. Racz, the procedure has become a key option for patients with post-laminectomy syndrome, lumbar radicular pain, and adhesive epiduritis who have not responded to conventional epidural injections.
Central to this technique is the Racz® Catheter—a spring-wound, radiopaque epidural catheter created under the direction of Dr. Gabor Racz to safely navigate fibrotic areas and deliver targeted therapy into the anterior-lateral epidural space.
Why use the Racz Catheter?
The Racz Catheter was developed to address a specific challenge: accessing the epidural space in patients with dense scar tissue, particularly after surgery. Its features make it ideal for effective and safe adhesiolysis:
- Flexible, non-traumatic tip for navigating around nerve structures with minimal risk of injury
- Radiopaque spring-wound body for enhanced fluoroscopic visibility
- Bend and depth markers for controlled, accurate advancement
- Stimulation-compatible to confirm correct catheter placement
How does the Racz Catheter Support Different Access Approaches?
One of the advantages of using the Racz Catheter is its ability to support a variety of access approaches, each suited to different types of adhesions and patient anatomy. Choosing the right approach helps optimize results based on the patient’s anatomy and the location of the adhesions.
- Caudal Approach – Ideal for lumbar fibrosis and post-laminectomy cases. The catheter’s flexibility allows smooth advancement through rigid fibrotic areas.
- Interlaminar Approach – Best for central or midline pathology. Enhanced visibility supports precise catheter placement.
- Transforaminal Approach – Effective for lateral or foraminal adhesions. The steerable tip allows targeted treatment of hard-to-reach regions.
Each approach can be tailored to the patient’s specific clinical presentation, allowing for more effective and focused therapy.
Technical Considerations and Best Practices
Mastering this technique requires attention to detail, patient safety, and a thorough understanding of the catheter’s capabilities. Insights from the Racz EUD Library and Dr. Racz highlight several key recommendations:
Choose the Right Tool
The plastic-coated, spring-tipped epidural Racz catheter provides fluoroscopic visibility, safe navigation with a soft tip, and durability against kinking. Its design allows multiple passes through the same needle without risk of shearing, ensuring precise and safe adhesiolysis.
Correct Catheter Placement
While early techniques targeted the posterior epidural space, experience showed that scar tissue often limited access. Directing the catheter into the anterior-lateral epidural space—particularly at the L3 nerve root via the sacral hiatus—improves therapeutic reach and effectiveness in complex post-surgical cases
Follow Pre and Post Procedure Protocol
A thorough diagnostic workup, including history, physical exam, and imaging, is essential before neuroplasty. Patients should be screened for psychological factors and committed to multidisciplinary rehabilitation. Post-procedure, physical therapy, stretching, and exercise help maintain nerve mobility, blood supply, and long-term recovery.
Access Needle Selection in the Racz Procedure
While the catheter performs the therapeutic portion of epidural neuroplasty, precise access to the epidural space is foundational to the success of the Racz Procedure. The characteristics of the access needle determine the trajectory, steering capability, and ultimate placement of the Racz® Catheter within an anatomically complex or fibrotic epidural compartment.
The RX-2 Coudé® Needle, created under the direction of Dr. Gabor Racz, is frequently used in adhesiolysis because its curved, directional bevel provides predictable control when advancing the catheter toward: the anterior epidural space, the symptomatic side, and the targeted nerve root level.
Directional access is particularly important in patients with post-surgical fibrosis, where posterior scarring can restrict catheter advancement and block medication spread.
Interested in continuing to learn about this technique and mastering the procedure? Visit the Racz Library at Racz EDU to gain insights from expert lectures and videos related to this topic.
FAQs: Adhesiolysis with Racz® Catheter
Q1: Can the Racz Catheter be used for spinal levels other than lumbar?
Yes, it can be used in cervical and thoracic spine areas, with approaches adapted to the patient’s condition.
Q2: Is fluoroscopic guidance required for using the Racz Catheter?
Yes, fluoroscopy ensures accurate catheter placement and safe adhesiolysis.
Q3: Can adhesiolysis with the Racz Catheter be repeated if pain returns?
Yes, adhesiolysis procedures can be repeated if symptoms persist or return over time. Since scar tissue can redevelop, some patients may benefit from staged treatments to maintain pain relief and improve function.
 Sign in
Sign in
 Create Account
Create Account